Vital Signs Are Not Just Numbers
Date published: July 1, 2025
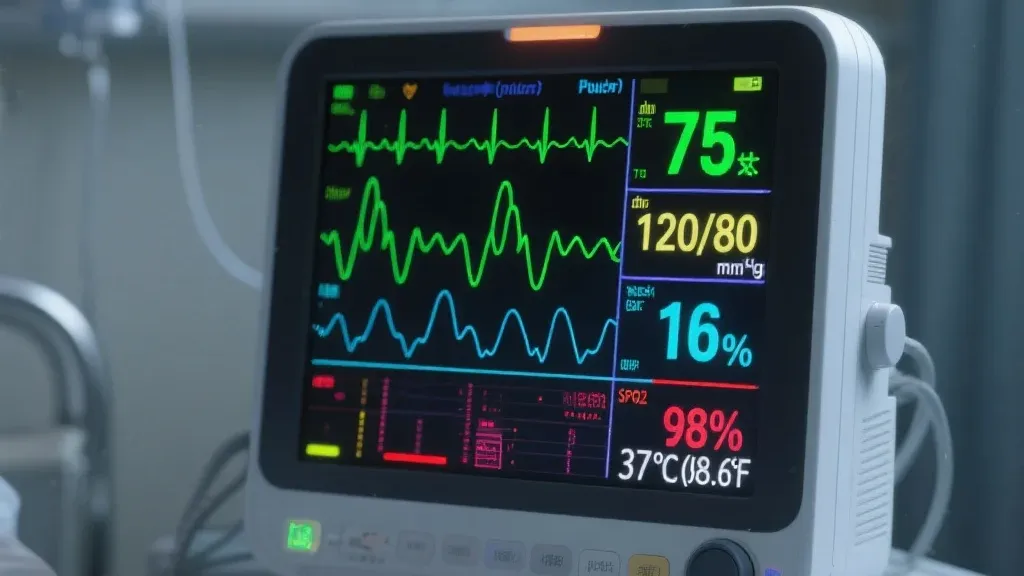
Respirations: 24.
O2 saturation: 92%.
Pulse: 99. BP: 100/60.
Most charts would call that “stable.”
But the body is whispering a story.
It’s easy to miss. On paper, it looks fine. “Within range.” “No critical alerts.” But if you’ve been at the bedside long enough, you know the feeling that quiet pattern that doesn’t sit right. The patient who’s breathing faster. Whose skin looks a little cooler. Whose blood pressure is technically okay but trending downward.
In early decline, nothing screams. It suggests. And unless we train nurses to hear that suggestion to understand what “not quite right” feels like we’ll keep catching deterioration too late.
This is why I believe vital signs are not just numbers. They’re narratives. And how we teach nurses to read them both analytically and intuitively directly determines who gets rescued in time.
The Problem with “Within Normal Limits”
Too often, nurses are taught to view vitals as isolated data points. We see numbers. We write them down. We move on. But what if the respiratory rate has been creeping up for the past six hours? What if that O2 sat was 97% yesterday, and now it’s barely 92% on the same amount of oxygen? What if the patient suddenly doesn’t want to eat and seems more withdrawn?
Alone, none of those facts sound the alarm. But together, they form a signal. One that says: pay attention now before it’s too late.
In my decades of practice and education, I’ve seen far too many situations where deterioration was only recognized after the patient crashed. Nurses had noticed something but didn’t feel empowered to name it, to escalate it, to act on it.
And so the patient coded. Or seized. Or was transferred to the ICU hours after the first clues appeared.
What We Should Be Teaching Instead
At Lifebeat Solutions, we built our Mastering Vital Signs course around one core belief: pattern recognition saves lives. It’s not enough to know the normal ranges.
Nurses need to:
Spot early deviations, even when they’re subtle
Understand what different combinations of vitals actually mean
Recognize when “normal” isn’t really normal for that patient
Speak up with clarity, not just concern
We teach nurses how to ask critical questions in real time:
What does a rising respiratory rate mean in this clinical picture?
How do subtle BP changes forecast perfusion collapse?
When should “normal” vital signs still prompt a rapid response call?
Because early warning doesn’t come from protocols alone. It comes from clinical judgment. From trends. From confidence.
And confidence is built not born.
Why This Matters Now
We are in a time of extraordinary pressure on nurses. New grads are being rushed into high-acuity units. Experienced nurses are managing double the patient load. Fatigue is high. Resources are low. And under those conditions, it’s easy to become reactive instead of reflective.
But in acute care, reflection is prevention.
If we want to reduce failure to rescue, we must shift how we approach basic nursing assessments. We need to move from “checking vitals” to interpreting them. From inputting numbers to communicating risk.
This is not extra work. It’s essential work.
And the payoff is real fewer missed deteriorations, safer handoffs, more timely interventions, and ultimately, lives saved.
What I Tell Every Nurse I Teach
You don’t have to be a critical care expert to catch early decline. But you do have to be curious. You do have to notice. And you have to be willing to say, “Something doesn’t feel right,” even when the chart looks fine.
Because no monitor or alert system will ever replace the instincts of a present, trained, and empowered nurse.
If you’re a hospital leader or educator ask yourself:
Are your nurses trained to interpret patterns, or just record data?
Do they feel safe to speak up when the numbers “don’t look wrong” but feel off?
Have you built a culture where intuition is respected and followed up on?
If not, you may be missing the single greatest tool in your safety arsenal: the vigilance of the nurse.
At Lifebeat Solutions, we help hospitals reduce harm by teaching nurses how to recognize what’s coming before the patient crashes.
📘 Our Mastering Vital Signs course builds that confidence one data point, one decision at a time. 📗 Learn more: https://lifebeatsolutions.com
#EarlyWarningSigns #VitalSignsTraining #NurseAssessment #PatientDeterioration #LifebeatSolutions #ClinicalJudgment #NursingEducation
Vital Signs Are Not Just Numbers
Date published: July 1, 2025
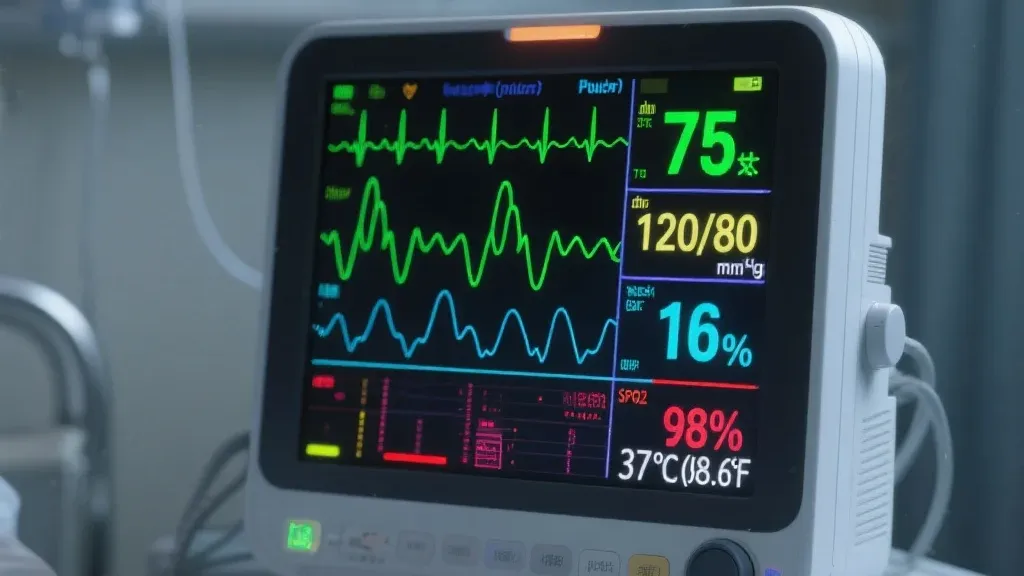
Respirations: 24.
O2 saturation: 92%.
Pulse: 99. BP: 100/60.
Most charts would call that “stable.”
But the body is whispering a story.
It’s easy to miss. On paper, it looks fine. “Within range.” “No critical alerts.” But if you’ve been at the bedside long enough, you know the feeling that quiet pattern that doesn’t sit right. The patient who’s breathing faster. Whose skin looks a little cooler. Whose blood pressure is technically okay but trending downward.
In early decline, nothing screams. It suggests. And unless we train nurses to hear that suggestion to understand what “not quite right” feels like we’ll keep catching deterioration too late.
This is why I believe vital signs are not just numbers. They’re narratives. And how we teach nurses to read them both analytically and intuitively directly determines who gets rescued in time.
The Problem with “Within Normal Limits”
Too often, nurses are taught to view vitals as isolated data points. We see numbers. We write them down. We move on. But what if the respiratory rate has been creeping up for the past six hours? What if that O2 sat was 97% yesterday, and now it’s barely 92% on the same amount of oxygen? What if the patient suddenly doesn’t want to eat and seems more withdrawn?
Alone, none of those facts sound the alarm. But together, they form a signal. One that says: pay attention now before it’s too late.
In my decades of practice and education, I’ve seen far too many situations where deterioration was only recognized after the patient crashed. Nurses had noticed something but didn’t feel empowered to name it, to escalate it, to act on it.
And so the patient coded. Or seized. Or was transferred to the ICU hours after the first clues appeared.
What We Should Be Teaching Instead
At Lifebeat Solutions, we built our Mastering Vital Signs course around one core belief: pattern recognition saves lives. It’s not enough to know the normal ranges.
Nurses need to:
-Spot early deviations, even when they’re subtle
-Understand what different combinations of vitals actually mean
-Recognize when “normal” isn’t really normal for that patient
-Speak up with clarity, not just concern
We teach nurses how to ask critical questions in real time:
-What does a rising respiratory rate mean in this clinical picture?
-How do subtle BP changes forecast perfusion collapse?
-When should “normal” vital signs still prompt a rapid response call?
Because early warning doesn’t come from protocols alone. It comes from clinical judgment. From trends. From confidence.
And confidence is built not born.
Monitoring and Reporting
Collecting and analyzing data on safety incidents to identify trends and areas for improvement.
Establishing Standards
Developing and enforcing safety protocols to ensure consistency and quality across healthcare organizations.
Promoting Education
Providing training and resources to healthcare professionals to enhance their knowledge and skills in patient safety.
Encouraging Transparency
Creating a culture where healthcare workers feel empowered to report errors and near-misses without fear of retribution.

Driving Innovation
Leveraging technology and research to implement cutting-edge solutions for patient safety challenges.

Why This Matters Now
We are in a time of extraordinary pressure on nurses. New grads are being rushed into high-acuity units. Experienced nurses are managing double the patient load. Fatigue is high. Resources are low. And under those conditions, it’s easy to become reactive instead of reflective.
But in acute care, reflection is prevention.
If we want to reduce failure to rescue, we must shift how we approach basic nursing assessments. We need to move from “checking vitals” to interpreting them. From inputting numbers to communicating risk.
This is not extra work. It’s essential work.
And the payoff is real fewer missed deteriorations, safer handoffs, more timely interventions, and ultimately, lives saved.
What I Tell Every Nurse I Teach
You don’t have to be a critical care expert to catch early decline. But you do have to be curious. You do have to notice. And you have to be willing to say, “Something doesn’t feel right,” even when the chart looks fine.
Because no monitor or alert system will ever replace the instincts of a present, trained, and empowered nurse.
If you’re a hospital leader or educator ask yourself:
Are your nurses trained to interpret patterns, or just record data?
Do they feel safe to speak up when the numbers “don’t look wrong” but feel off?
Have you built a culture where intuition is respected and followed up on?
If not, you may be missing the single greatest tool in your safety arsenal: the vigilance of the nurse.
At Lifebeat Solutions, we help hospitals reduce harm by teaching nurses how to recognize what’s coming before the patient crashes.
📘 Our Mastering Vital Signs course builds that confidence one data point, one decision at a time. 📗 Learn more: https://lifebeatsolutions.com
#EarlyWarningSigns #VitalSignsTraining #NurseAssessment #PatientDeterioration #LifebeatSolutions #ClinicalJudgment #NursingEducation
